
Once swelling has lessened, compression garments, such as sleeves and stockings, can help prevent new fluid accumulation.
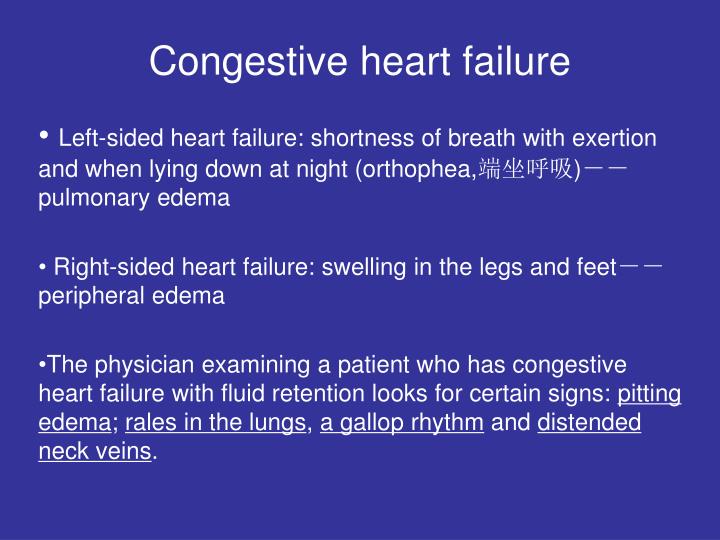
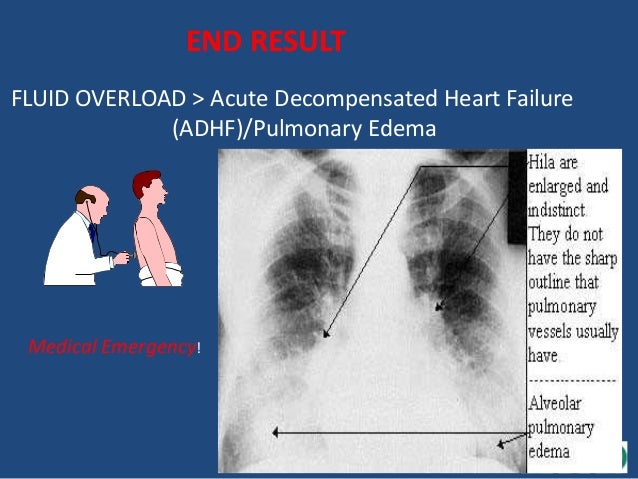
So does spending time with the affected limbs elevated above the heart. Exercise, particularly involving the affected limbs, can help veins return blood to the heart. These types of edema cannot be cured, so the goal is management. The back-up of blood from these conditions causes pressure, which forces fluid from tiny capillaries in the area and into the surrounding tissues. It’s an uphill journey from the extremities to the heart, and venous insufficiency allows the blood to pool.Įdema is also a symptom of congestive heart failure, a progressive condition in which the heart becomes unable to pump enough blood to meet the body’s needs. This is when age, illness, injury or the side effects of medications cause the veins and the valves within them to be less efficient at returning blood to the heart. Edema can also cause abdominal swelling, shortness of breath, elevated heart rate and chest pain.Ī common cause of edema in older adults is venous insufficiency. Severe edema causes a condition known as pitting, which is when pressure applied to the swollen area causes an indentation that is slow to fade.
#Fluid retention congestive heart failure skin
Symptoms include visible swelling or puffiness and skin that looks tight and shiny. It occurs when fluid becomes trapped in the affected tissues.Įdema can occur in any part of the body, and it shows up most commonly in the ankles, feet, legs and hands. I know I’m not the only senior affected by edema, and I hope you might consider devoting a column to it.ĭear Reader: You’re correct that many older adults experience edema, which is the medical term for swelling. Now I have been diagnosed with early-stage congestive heart failure. Ī ventricular assist device (bridge to transplant or as a destination therapy) or cardiac transplant is reserved for those with severe disease despite all other measures.Dear Doctor: I am a 76-year-old man who has dealt with edema in various intensities for several years. Most patients who satisfy the criteria for cardiac resynchronization therapy implantation are also candidates for an implantable cardioverter-defibrillator and receive a combined device. Cardiac resynchronization therapy with biventricular pacing can improve symptoms and survival in selected patients who are in sinus rhythm and have a reduced left ventricular ejection fraction and a prolonged QRS duration. ĭevice therapy: Implantable cardioverter-defibrillator (ICD) is used for primary or secondary prevention of sudden cardiac death. In African-Americans, hydralazine plus oral nitrate is indicated in patients with persistent NYHA class III to IV HF and LVEF less than 40%, despite optimal medical therapy (beta-blocker, angiotensin-converting enzyme inhibitors, ARB, aldosterone antagonist (if indicated), and diuretics. Angiotensin receptor neprilysin inhibitors should not be given within 36 hrs of angiotensin-converting enzyme inhibitors dose. Diuretic therapy is mainly used for symptom control. More limited evidence of survival benefit is available for diuretic therapy. Improved patient survival has been documented with the use of beta-blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor neprilysin inhibitor, hydralazine plus nitrate, and aldosterone antagonists. Combination therapy with these agents improves outcomes and reduces hospitalizations in patients with HF. Diuretics, beta-blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, angiotensin receptor neprilysin inhibitor, hydralazine plus nitrate, digoxin, and aldosterone antagonists can produce an improvement in symptoms and are indicated for patients with HF based on their functional classification and severity of symptoms.


 0 kommentar(er)
0 kommentar(er)
